Prostate cancer is the third most prevalent cancer among men in Hong Kong, with approximately 40% of diagnosed patients identified at stages one or two. Traditional treatment options often involve whole-organ approaches, such as prostatectomy or radiation therapy, which can lead to side effects that affect urinary, sexual, and rectal functions, thereby compromising quality of life. In recent years, the medical community has begun to explore focal therapies, which focus on organ preservation and the targeted elimination of cancer cells with patients recovering swiftly and experiencing no postsurgical side effects.
Prostate Cancer Cases Surge Significantly
According to the latest data from the Hospital Authority, Hong Kong recorded 2,758 new cases of prostate cancer in 2022, making it the third most common cancer among men and ranking fourth in male cancer mortality. Compared to other common cancers, prostate cancer has shown a significant increase, with a cumulative growth of 69.1% from 2012 to 2022.
Prostate cancer staging is typically classified intro four stages based on tumor size (T), lymph node involvement (N), and metastasis to other organs (M). Approximately 38% of new patients are diagnosed at stage one or two, indicating that the tumor has not yet spread beyond the prostate.
Traditional Treatments and Challenges
The treatment options for prostate cancer depend on the activity level and extent of the cancer cells. Some cancer cells grow slowly, while others are more aggressive. Therefore, when formulating a treatment plan, multiple factors must be considered, including age, health status, cancer stage, life expectancy, patient preferences, as well as the levels and rate of increase of prostate-specific antigen (PSA) and the Gleason score. A higher Gleason score indicates a faster growth and a higher risk of spreading for prostate cancer.
For different stages of prostate cancer, treatment plans vary. For stage one and two, options typically include active surveillance (regular blood tests and biopsies) or whole-organ treatments such as radical prostatectomy or radiation therapy. Stage three may require a radical prostatectomy along with pelvic lymph node removal or the option of radiation therapy. Treatment for stage four includes hormone therapy, chemotherapy, newer oral hormone inhibitors, and radiation therapy. However, traditional whole-organ treatments can lead to side effects affecting urination, sexual function, and rectal health, which may impact the patient's quality of life.
New Direction in Prostate Cancer Treatment: Focal Therapy
In recent years, robotic-assisted minimally invasive prostatectomy has become common. The precision of needle placement and suturing has improved, reducing the risk of bleeding and complications for patients. By utilizing clear imaging to enhance surgical detail, important nerves and blood vessels can be preserved, thereby increasing patient safety and improving postoperative outcomes.
With the rise of personalized cancer treatment, significant breakthroughs have emerged in the management of prostate cancer. Focal therapy are now available for suitable patients, allowing for the preservation of the prostate and its functions. Focal treatment targets tumors confined to the prostate (usually on one side) without spreading to other tissues or organs. The goal is to destroy cancer cells while preserving healthy tissue, thereby reducing side effects and complications.
Currently, there are several focal treatment methods available, including High-Intensity Focused Ultrasound (HIFU), Cryoablation, Microwave Ablation, and Irreversible Electroporation (IRE). IRE can effectively destroy targeted tissue without using heat, making it safe for application near critical structures while minimizing long-term damage. Additionally, the procedure is quicker compared to other methods.
IRE: A New Treatment Technique
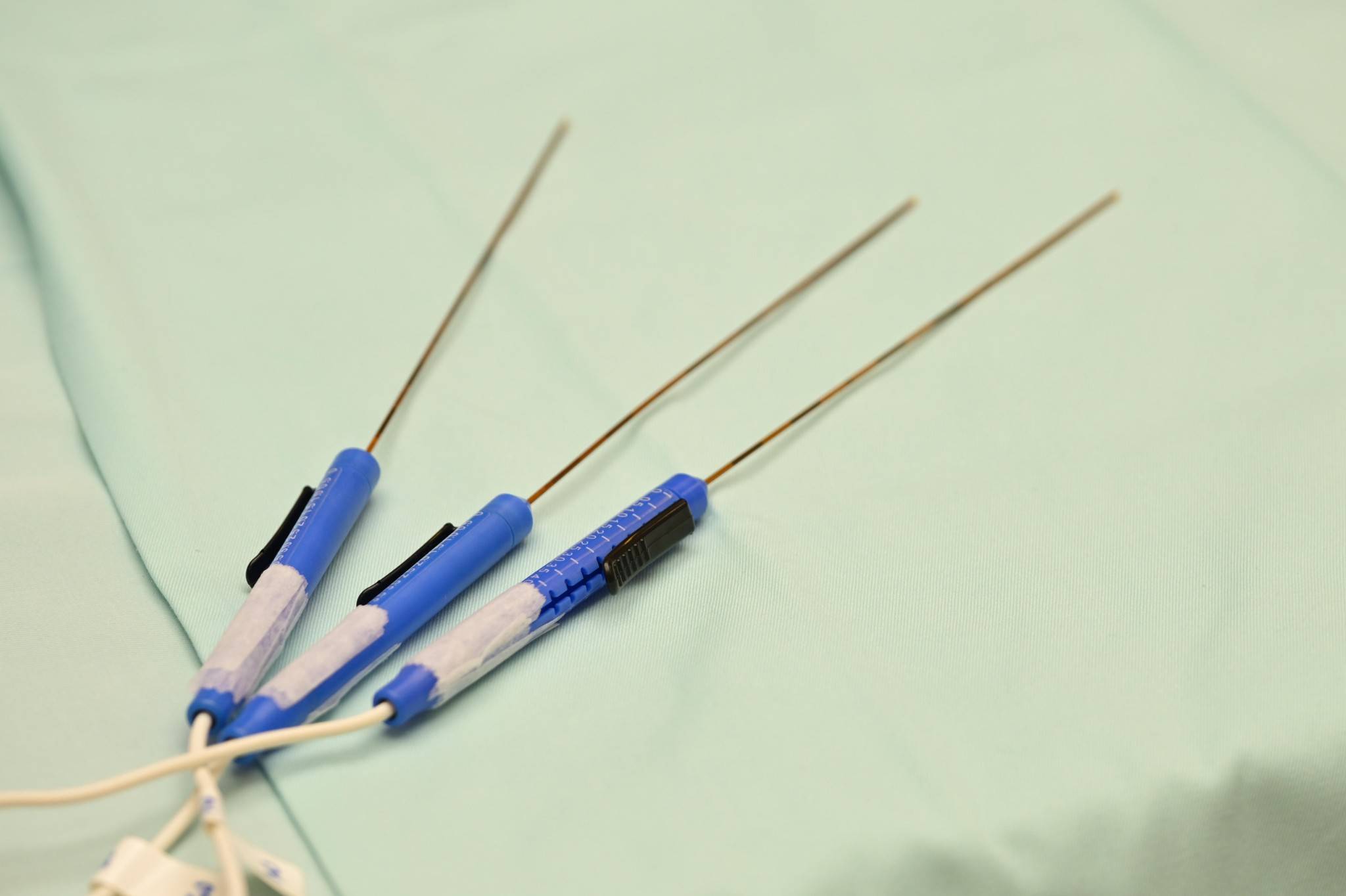
Irreversible Electroporation (IRE) involves inserting several electrode needles through the skin to surround cancer cells, allowing electric currents to pass through the cancer cells without damaging blood vessels or nerves. This process creates pores in the cancer cell membranes, disrupting their internal balance and preventing normal function, leading to gradual cell death. IRE's unique advantage over other focal treatments is its non-thermal, non-freezing nature, which effectively preserves the integrity of surrounding critical structures and eliminates the risk of thermal spread (the phenomenon where blood flow carries away heat, reducing treatment effectiveness on nearby cancer cells). During the procedure, ultrasound is used for real-time monitoring to ensure cancer cells are destroyed.
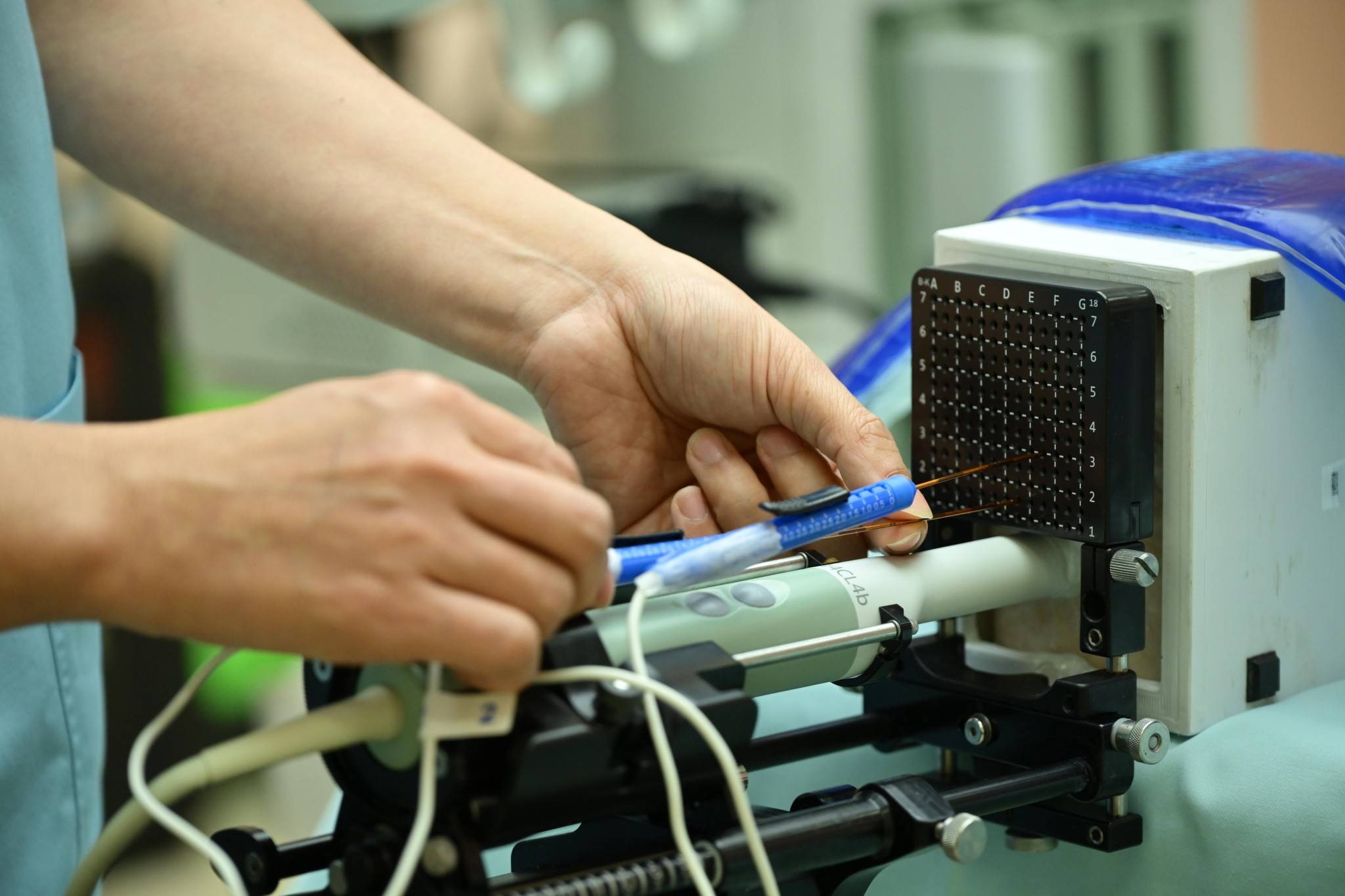
In the surgical process, needles are placed to target the tissue. Typically, two electrodes are activated at a time, but four to six electrodes are generally used in each case to ensure comprehensive coverage of the cancer cells. Once the electrodes are positioned, the doctor initiates electrical pulses to destroy the cancer cells. The surrounding healthy prostate tissue remains intact, avoiding damage. The surgery takes approximately 1 to 1.5 hours, and the catheter is usually removed within 24 hours postoperation, allowing normal urination without any risk of incontinence. Patients can typically return home within one to two days after the procedure.
Only 4.1% severe side effects
A large study conducted in the United States in 2024 has shown that IRE has minimal severe side effects at only 4.1%, with no cases of urinary incontinence, and 90.1% of patients maintaining erectile function within 90 days post-operation. The U.S. Food and Drug Administration also approved this technology for prostate tissue ablation treatment in December 2024, and it has received CE certification from the European Union.
By combining robotic-assisted surgery with IRE, doctors can select the most suitable treatment plan tailored to each patient's specific circumstances, achieving true personalized care. Different treatment options come with varying levels of effectiveness, side effects, and risks. Therefore, patients should discuss their choices thoroughly with their primary physician to determine the best treatment approach for their individual needs.