Types and Causes of Knee Arthritis (February, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 1)
Just as machines can wear out, the human body's joints are also susceptible to deterioration. Knee osteoarthritis is a common problem that afflicts many middle-aged and elderly individuals. Among the various joints in the body, the knee is one of the most frequently affected by degenerative changes. Activities such as walking, running, and hiking all rely heavily on the knees. Knee problems can significantly impact a patient's daily life.
According to a 2001 survey by the Chinese University of Hong Kong, the incidence rate of knee osteoarthritis in Hong Kong is equally high as in Western countries. The prevalence of knee arthritis increases rapidly in women after menopause. Among men aged 50 or above, 17% have experienced persistent knee pain, and 7% have been diagnosed with knee arthritis. For women in the same age group, 24% suffer from persistent knee pain, and 13% have been diagnosed with knee arthritis.
Understanding the Knee
First, we need to understand the structure of the knee. The knee is primarily composed of three parts: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). The knee is surrounded by multiple soft tissues, including the joint capsule, tendons, and muscles. On the surfaces where the femur and tibia meet, there is a layer of 2-3 millimeters of articular cartilage. Additionally, there are two menisci (crescent-shaped cartilage discs) between the two bones, which are soft and smooth, serving to cushion and stabilize the knee. These cartilaginous structures are the primary areas affected in arthritis.
Types and Causes of Knee Arthritis
There are various causes of knee arthritis, such as degenerative osteoarthritis, rheumatoid arthritis, gouty arthritis and post-traumatic arthritis. Osteoarthritis is the most common type among all different type of arthritis. While the exact cause of osteoarthritis is still unknown to the medical community, most experts believe that factors such as aging and injury can lead to different degrees of cartilage wear and tear. Regarding risk factors, studies have shown that obese individuals are 5 times or more likely to develop knee arthritis compared to those with normal weight. If a patient has previously sustained a knee injury (e.g., cruciate ligament tear, meniscus injury, or fracture), the risk of developing knee arthritis increases 7-fold compared to those without prior injury.
This article was written by Dr. Cheung Man Hong, a consultant in Orthopaedics & Clinical Director Of Robotic Surgery (Joint Replacement) at the Hong Kong Adventist Hospital - Stubbs Road
Osteoarthritis vs. Rheumatoid Arthritis (March, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 2)
Knee Osteoarthritis
Osteoarthritis is the most common type of joint disease. Almost any joint can develop osteoarthritis, but it most often affects weight-bearing joints like the knees, hips, spine, first metatarsophalangeal joint (base of the big toe), and first carpometacarpal joint (base of the thumb). Among these, knee osteoarthritis is commonest type of osteoarthritis.
In the early stages, the cartilage on one side (medial or lateral) of the joint may start to wear down, and gradually progresses to the other side. Eventually, the cartilage lining the joint may become almost completely eroded. X-ray examinations can reveal that the normally smooth joint surface becomes uneven, with bone overgrowth, commonly known as bone spurs. Many people mistakenly think the pain is caused by the bone spurs rubbing against the soft tissue, but this is not the case. The main cause of the pain is actually the wear and tear of the cartilage. Even if the bone spurs are removed, the pain may not improve significantly.
Key Symptoms
In the early stage, patients may feel knee pain when going up/down stairs or walking on slopes, accompanied by joint swelling. Abnormal grinding noises may be heard when moving the joint. In the late stage, patients may experience joint stiffness, difficulty in bending/extending the joint, and even deformities like "bow legs." The range of motion decreases, making the patient difficult to climb stairs or squat. These symptoms not only cause inconvenience in work and daily life, but may also affect the patient's emotional well-being.
Osteoarthritis vs. Rheumatoid Arthritis
Many people confuse osteoarthritis with rheumatoid arthritis, as they share some similar symptoms like joint pain, redness, and swelling. However, the underlying causes and treatment approaches are completely different. There are also other conditions like gout or pseudogout, where uric acid or calcium crystals deposit in the joint, leading to acute, severe joint pain and swelling, which can resemble osteoarthritis symptoms. Therefore, if a patient experiences frequent joint pain and swelling, they should seek medical attention promptly to determine the root cause and receive appropriate treatment.
This article was written by Dr. Cheung Man Hong, a consultant in Orthopaedics & Clinical Director Of Robotic Surgery (Joint Replacement) at the Hong Kong Adventist Hospital - Stubbs Road
How to Diagnose Knee Disease (April, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 3)
How to diagnose?
The doctor will first inquire about the patient's medical history and family history, particularly asking about the timing and triggering factors of the joint pain. For example, if the patient has osteoarthritis, the pain usually worsens after using the joint (walking, moving, or climbing stairs), but improves with rest. In contrast, if the patient has rheumatoid arthritis, the joints are often more painful in the morning upon waking up, and the pain tends to ease after some movement. If the patient experiences knee joint swelling and pain after consuming seafood, internal organs, or alcohol, the possibility of gout should be considered. The doctor will also assess the severity of the arthritis based on the patient's mobility (e.g., whether a cane or walker is needed) and the frequency of pain medication use.
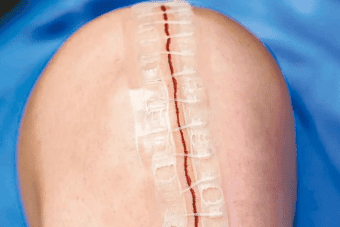
After the interview, the doctor will conduct a thorough physical examination, paying particular attention to the location of knee pain, the patient's mobility, joint deformities, range of motion, lower limb muscle strength (such as the quadriceps), joint stability, and the structure and tension of related ligaments. If the patient is considering knee replacement surgery, the doctor will also examine the lower limbs, especially the condition of the feet, to check for any fungal infections (Tinea Pedis), as this would make the patient unsuitable for knee replacement surgery.
The doctor will then arrange an X-ray examination. Usually, the patient will be asked to adopt a standing posture when taking the knee X-ray, as the cartilage loss are often more apparent when the patient is standing compared to lying down. The X-ray will be checked for narrowing of the joint space and soft tissue swelling.
This article was written by Dr. Cheung Man Hong, a consultant in Orthopaedics & Clinical Director Of Robotic Surgery (Joint Replacement) at the Hong Kong Adventist Hospital - Stubbs Road
Bone Spurs (May, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 4)
Bone Spurs?
"Degenerative Osteoarthritis " is a condition that not everyone may have heard of, but I believe every Hong Kong citizen has heard of the so-called "bone spur" ailment affecting themselves or someone they know. Many patients discover they have knee pain, and after a X-ray examination, they are told that their knee has developed bone spurs, which is actually a misunderstanding.
A normal joint has a smooth overlying surface is smooth, but when the joint degenerate its surface becomes uneven. One contributing factor for the surface irregularly is the presence of bony outgrowths, which are commonly known as bone spurs. The emergence of bone spurs is the result of knee's surrounding tissues attempting to repair the degenerating knee. Bone spurs are most commonly seen in the knee. From X-rays, the bone spurs in a degenerative knee are often rounded bony protrusions around the joint, so these bone spurs are not sharp "spurs", and they will not pierce the soft tissues or skin to cause pain.
The main cause of a patient's knee pain is due to the wear and tear of the cartilage, as well as the accompanying bone loss, ligament laxity, joint capsule instability, synovial inflammation and swelling. The appearance of bone spurs is only a partial symptom of the degenerative knee, and not the primary culprit. Therefore, even if the bone spurs are removed, the pain will not improve significantly, so doctors will not perform surgery just to remove the bone spurs without addressing the underlying knee disease. In fact, the medical term for "bone spurs" is actually "osteophytes", meaning redundant bone growth.
However, the discovery of osteophytes on a knee X-ray does have its significance. If the patient has symptoms of knee arthritis, the presence of osteophytes is one of the indicators used by doctors to analyze the severity of knee degeneration. Pathologically, osteophytes can compress or tighten the knee capsule or ligaments, limiting the range of knee motion, and even leading to knee deformity. If the patient's knee degeneration is severe and requires joint replacement surgery, the surgeon must remove all osteophytes during the procedure in order to restore the balance of soft tissue and ligament tension, as well as improve the patient's knee joint mobility.
This article was written by Dr. Cheung Man Hong, a consultant in Orthopaedics & Clinical Director Of Robotic Surgery (Joint Replacement) at the Hong Kong Adventist Hospital - Stubbs Road
Treatment for Knee Osteoarthritis (June, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 5)
Overview of Treatment Methods
The treatment for knee osteoarthritis can be divided into several aspects: non-surgical treatment (including drug therapy and non-drug therapy) and surgical treatment.
Non-drug treatment
For patients with relatively mild symptoms, X-rays showing the knee has not reached severe degeneration, and without significant knee deformity and knee stiffness, doctors generally will first consider non-surgical treatment options. The principles and goals of non-surgical treatment are as follows:
- Reduce further joint wear
- Slow down the developement of complication of osteoarthritis
- Alleviate the symptoms of osteoarthritis, such as pain
- Maintain and improve the joint mobility
- Strengthen the leg muscles
According to the clinical guidelines of the American Academy of Orthopedic Surgeons, the effective non-drug treatment methods proven by clinical studies include weight management and effective physical therapy and training.
Weight management
Many people think weight control is a cliche, but in fact, there is a large amount of medical literature that proves that for patients with a body mass index (BMI) above 25, weight control can effectively relieve pain, and is even more effective than medication. Because weight control is one of the important factors that can reduce the burden on the knee, it is an effective way to reduce further joint wear. To maintain a normal weight index, you must learn to start from diet, exercise, and emotional support in order to achieve an ideal and healthy weight management.
Exercise and physical therapy
Many patients think that since they already have knee degeneration and overuse, continuing to exercise will accelerate the overuse and degeneration. So should they do more exercise or reduce activity to protect the joint? The answer is that they should continue to exercise, and even strengthen their training. In fact, lack of exercise in the knee and lower limbs will cause muscle loss. If there is muscle atrophy, they cannot support the knee, making the knee unstable, and increasing the pressure on the cartilage and related soft tissues, and thus further aggravating the degeneration. In simple terms, the less you move, the more it hurts.
This article was written by Dr. Cheung Man Hong, a consultant in Orthopaedics & Clinical Director Of Robotic Surgery (Joint Replacement) at the Hong Kong Adventist Hospital - Stubbs Road
Exercises Suitable for Patients with Knee Joint Degeneration (August, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 6)
Shouldn't people with joint degeneration exercise? Will it worsen the condition?
Many patients believe that if they have knee joint degeneration and wear and tear, they should avoid exercise and let their joints rest more. In fact, this approach is counterproductive because knee joint degeneration is closely related to muscle atrophy in the legs. Lack of exercise will only weaken the muscles further, potentially accelerating joint degeneration.
In reality, exercise is an indispensable and even the most effective treatment for osteoarthritis. Medical research has proven that regular exercise can effectively alleviate pain, reduce the need for pain medication, and enhance joint mobility. Many patients with knee joint degeneration can cycle, swim, and perform muscle strengthening exercises with almost no pain. Generally speaking, low-impact exercises that put less stress on the joints, such as swimming and cycling, are prioritized.
Exercises Suitable for Patients with Knee Joint Degeneration
In general, we recommend that patients consider three types of exercises: i. Joint and muscle stretching exercises, ii. Muscle strengthening exercises and balance training, and iii. Aerobic exercises.
Joint and muscle stretching exercises involve movements that significantly mobilize the joints, helping to keep the joints functioning smoothly and alleviating stiffness and pain. Patients can adopt different positions, such as lying down, sitting, or standing, while alternately flexing the knee joint as much as possible.
Muscle stretching exercises, also known as stretching exercises, help improve the flexibility of the muscles and tendons, preventing cramps and post-exercise muscle soreness. The most common stretching exercise involves the hamstring stretch: the patient sits on the edge of the bed, alternately placing each foot on the bed while keeping the back straight and attempting to keep the knee joint straight. Then, they reach forward toward their toes and apply downward pressure on the knee joint until they feel a stretch in the hamstrings and the back of the knee, maintaining the position for 10 seconds before relaxing. Many patients with knee joint degeneration may experience stiffness that prevents the knee from fully straightening, along with frequent cramps or discomfort in the back of the thigh or knee. This training can improve the flexibility of the hamstrings and tendons and help address the issue of the knee joint not fully straightening.
Muscle Strengthening Exercises (September, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 7)
Muscle Strengthening Exercises
For the knee joint, one of the most important muscles is the quadriceps located above the knee. The quadriceps is one of the largest muscles in the human body and consists of four muscle groups: the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius. These muscles are located on the front side of the thigh and attach to the iliac bone of the pelvis, the femur, and the patella. The function of the quadriceps is to contract, pulling on the tendons over the knee to extend the knee and lift the leg, maintaining an upright posture and supporting the body. This muscle is essential for activities such as walking, running, and climbing stairs.
For patients beginning to experience knee joint degeneration, one of the first symptoms is often pain, soreness, and weakness when going up and down stairs. One important factor contributing to this is insufficient strength in the quadriceps. Therefore, strengthening and maintaining the strength of the quadriceps is crucial for patients with knee joint degeneration. In fact, even after undergoing joint replacement surgery, having strong quadriceps can lead to faster recovery of function post-operatively.
For elderly patients or those with more severe joint degeneration, simple quadriceps training can be started. Here, I will introduce two types of exercises: First Exercise: The patient lies flat on their back with a towel placed 6 to 7 inches under the knee. They should press the back of the knee down toward the bed, hold for 10 seconds, and then relax. Repeat this about 10 times before switching sides to repeat the exercise. Second Exercise: This exercise can be performed in two positions. The patient can lie flat on their back and tie a 1 to 2-pound sandbag around the ankle joint. Then, they should slowly extend each leg alternately while maintaining the position for 5 to 10 seconds before slowly relaxing. As strength improves, they can gradually increase the weight and duration. If knee pain occurs while extending, the weight should be reduced. Patients can also choose to perform the training while sitting, again tying a 1 to 2-pound sandbag around the ankle joint and slowly extending the knee while maintaining the position for 5 to 10 seconds before relaxing.
For younger patients or those with less severe knee joint degeneration, they can engage in more advanced high-intensity training, which we will discuss in detail next time.
High-Intensity Training for Knee Joint Muscles (October, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 8)
For younger patients or those with less severe knee degeneration, more advanced high-intensity training can be undertaken:
Wall Squats
Start by standing with your back against a wall, feet shoulder-width apart. Slowly lower yourself as if sitting in an invisible chair, bending your knees to about 90 degrees. As you squat, engage your core and glutes, sliding down the wall until your thighs are parallel to the ground. Adjust your foot position to keep your knees above your ankles, maintaining your back flat against the wall. Hold this position for about 30 seconds to 1 minute. This exercise can improve knee joint stability and simultaneously strengthen the quadriceps, hamstrings, glutes, calves, and core muscles.
Calf Raises
Calf raises are primarily used to strengthen the calf muscles and enhance calf strength, providing shock absorption for the body. Stand upright with your feet flat on the ground, then shift your weight onto your toes and raise your heels as high as possible. Use your toe muscles to push your weight up and hold the calf muscles in a contracted position for 2-5 seconds before slowly lowering back to the starting position.
Single-Leg Squats
Single-leg squats effectively strengthen the muscles around the knee joint, significantly improving lower body muscle stability, balance, and coordination. Start by standing on one leg, extending your arms straight out in front of you at shoulder height and parallel to the floor. Lift the right leg off the ground, bend the left knee, and push your hips back, squatting as low as possible while maintaining your position. Then push yourself back to the starting position.
Knee Bridge
This exercise helps strengthen the glute muscles, enhancing glute strength and reducing the load on the knee joint. Begin by lying flat on your back on a mat, with your legs bent and your arms at your sides, palms facing down. Lift your hips until your knees, hips, and shoulders form a straight line, engaging your abdominal muscles. Hold this position for 2-3 seconds before slowly lowering your hips back down.
Medication Therapy (November, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 9)
In general, medication therapy has two main roles in treating knee osteoarthritis. The first role is when there is an acute flare-up of knee arthritis or severe joint pain; doctors will prescribe different types of pain relief and anti-inflammatory medications to alleviate the discomfort and pain associated with inflammation and swelling.
The most commonly used pain relief medication is paracetamol. Paracetamol is arguably the most widely used painkiller, but its analgesic effect is relatively modest. A study (Note 1) comparing the effects of paracetamol versus a placebo (a non-effective substance) found that 52% of those taking paracetamol reported reduced pain. Similarly, 51.9% of those in the placebo group also felt a reduction in pain. This suggests that the actual utility of pain relief medications may not be very significant. Nonetheless, doctors still consider it for treatment due to its high safety profile and long history of use. It may be a viable option for elderly patients or those with multiple health issues (such as poor kidney function).
Non-steroidal anti-inflammatory drugs (NSAIDs) are a class of anti-inflammatory painkillers that are generally more effective than paracetamol in alleviating pain. American Academy of Orthopaedic Surgeons guidelines also recommend considering them as a treatment option. However, these medications can lead to issues such as gastrointestinal bleeding and impaired kidney function, making them less suitable for older or higher-risk patients. When using NSAIDs, it might be advisable to combine them with gastric protectants to reduce associated side effects. Currently, many doctors also opt for newer generation medications like COX-2 inhibitors, which reduce the risk of gastrointestinal bleeding compared to traditional NSAIDs. However, they tend to be relatively expensive, and some clinical studies indicate that COX-2 inhibitors may increase the risk of cardiovascular diseases. Doctors must consider and balance the associated pros and cons when making their selections.
Another option is topical anti-inflammatory pain medications, such as pain relief creams and adhesive patches. The analgesic effect of topical medications is generally less effective than oral medications, but because the drugs are absorbed through the skin, they can reduce associated side effects. When using topical medications, it is important to monitor for any allergic reactions on the skin. If itching or redness occurs, they should not be continued. Additionally, do not use topical medications simultaneously with oral medications to avoid the risk of drug overdose.
1. Miceli-Richard C, Le Bars M, Schmidely N, Dougados M. Paracetamol in osteoarthritis of the knee. Ann Rheum Dis. 2004 Aug;63(8):923-30. doi: 10.1136/ard.2003.017236. PMID: 15249319; PMCID: PMC1755093.
Medication Therapy (December, 2024)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 10)
Last month, it was mentioned that medication therapy has two main roles in treating knee osteoarthritis. The first role is to use pain relief and anti-inflammatory medications during acute flare-ups of knee arthritis to alleviate discomfort caused by inflammation and swelling. The second role involves the long-term use of supplementary medications, hoping to reduce the progression of degeneration or even delay it.
Many citizens have high expectations for various nutritional supplements, bone supplements, or joint medications available in the market, believing that these can effectively control knee degeneration, protect the joints, or slow down degeneration. However, there is currently no large-scale medical data showing that any oral supplement can effectively delay the progression of degeneration fundamentally.
The most common oral supplements on the market are glucosamine and chondroitin. These two medications have a long history, with glucosamine being used in Europe and the United States for decades, proving to be very safe with almost no side effects. Some studies have shown that these two supplements have certain anti-inflammatory effects and can relieve pain. Various studies have also indicated that glucosamine or chondroitin can moderately alleviate short-term and medium-term pain, but most studies suggest that combining these two supplements offers no additional benefits. Furthermore, there is no evidence that either of these supplements, used alone or in combination, actually slows the degeneration process of arthritic joints or restores cartilage.
Although many people believe that traditional doctors overlook their interest in supplements, many doctors, including myself, are actually open to supplementary treatments. Therefore, it is generally recommended that patients try taking these supplements for several months to half a year; if there is no effect, they can consider stopping. It is also important not to neglect the significance of exercise and muscle training, which should be carried out simultaneously for better results. In recent years, many new types of supplements have been introduced in Hong Kong, such as collagen supplements, and I believe that large-scale studies are needed to confirm the effectiveness of these new medications.
In addition to oral supplements, another type of medication that attracts considerable attention from patients is various forms of injection therapy. This will be discussed in the next issue.
Joint Injection Therapy (January, 2025)
Published in the Hong Kong Economic Journal
The Latest Treatments and Developments for Knee Osteoarthritis (Part 11)
In addition to oral supplements, another type of medication that attracts considerable attention from patients is various forms of injection therapy, the most well-known being hyaluronic acid injections, commonly referred to as "gel injections" or "hyaluronic acid" in the market.
Hyaluronic acid is a glycosaminoglycan that naturally exists in the human body. It is widely distributed, particularly in high concentrations within synovial fluid in the joints. It is also present in the skin, nerves, and various connective tissues. In the knee joint, hyaluronic acid is a primary component of synovial fluid, which helps retain moisture and increases the viscosity of the synovial fluid, providing lubrication and preventing friction between bones during joint movement. Additionally, it is an important component of cartilage, enabling cartilage to retain moisture and exhibit its compression-resistant properties.
During the degeneration of joints, the synovial fluid within the joint may experience loss or degradation. Injecting hyaluronic acid into the joint cavity can help lubricate the joint and potentially stimulate cartilage cells to secrete new material to repair eroded cartilage. Currently, there are over ten types of joint fluid supplements available on the market, with varying injection amounts and frequencies ranging from a single injection to five injections. New formulations contain high molecular weight and highly cross-linked hyaluronic acid, requiring only a single injection for convenience, although they tend to be relatively expensive.
Regarding efficacy, a study published in the Hong Kong Medical Journal by the University of Hong Kong involved injecting hyaluronic acid into 95 patients with knee osteoarthritis, with an average age of 62, from October 2010 to May 2012. The average pain score before injection was 60 (with 100 being the most painful). Six weeks after the injection, the score decreased to 40, but one year later, it rose back to around 50. This suggests that the use of this injection is safe and effective in reducing joint pain, with a maximum effective duration of one year (clinically maintaining an average of 6 to 9 months).