Joint pain and stiffness may be related to joint degeneration and arthritis, which are common musculoskeletal diseases. The pain caused by these conditions can be uncomfortable and disruptive to daily life. In this article, we will analyze and understand osteoarthritis and its symptoms in depth, and explore how to alleviate joint pain.
What is Osteoarthritis?
Osteoarthritis, also known as degenerative joint disease or degenerative arthritis, is a degenerative disease caused by the long-term wear and tear of the cartilage that cushions the joints. This leads to inflammation, deformation, and abnormal bone spur growth. Osteoarthritis commonly affects weight-bearing joints such as the knees, hips, and fingers that are frequently used. The most common affected area is the knee joint.
Analyzing the Causes and Symptoms of Osteoarthritis
Causes of Osteoarthritis
Regarding the exact causes of osteoarthritis, the medical field has not yet reached a definitive conclusion. Most experts believe that factors such as aging and trauma can lead to varying degrees of cartilage wear and tear.
As for high-risk factors, different studies have shown that patients who are overweight have a 5-fold or even higher increased risk of developing knee osteoarthritis compared to people of normal weight. If a patient has previously had a knee injury (such as ACL tear, meniscus injury, fracture, etc.), the chance of developing knee osteoarthritis is increased by about 7 times compared to the general population.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis can generally be divided into early-stage and late-stage.
Early-stage Symptoms of Osteoarthritis
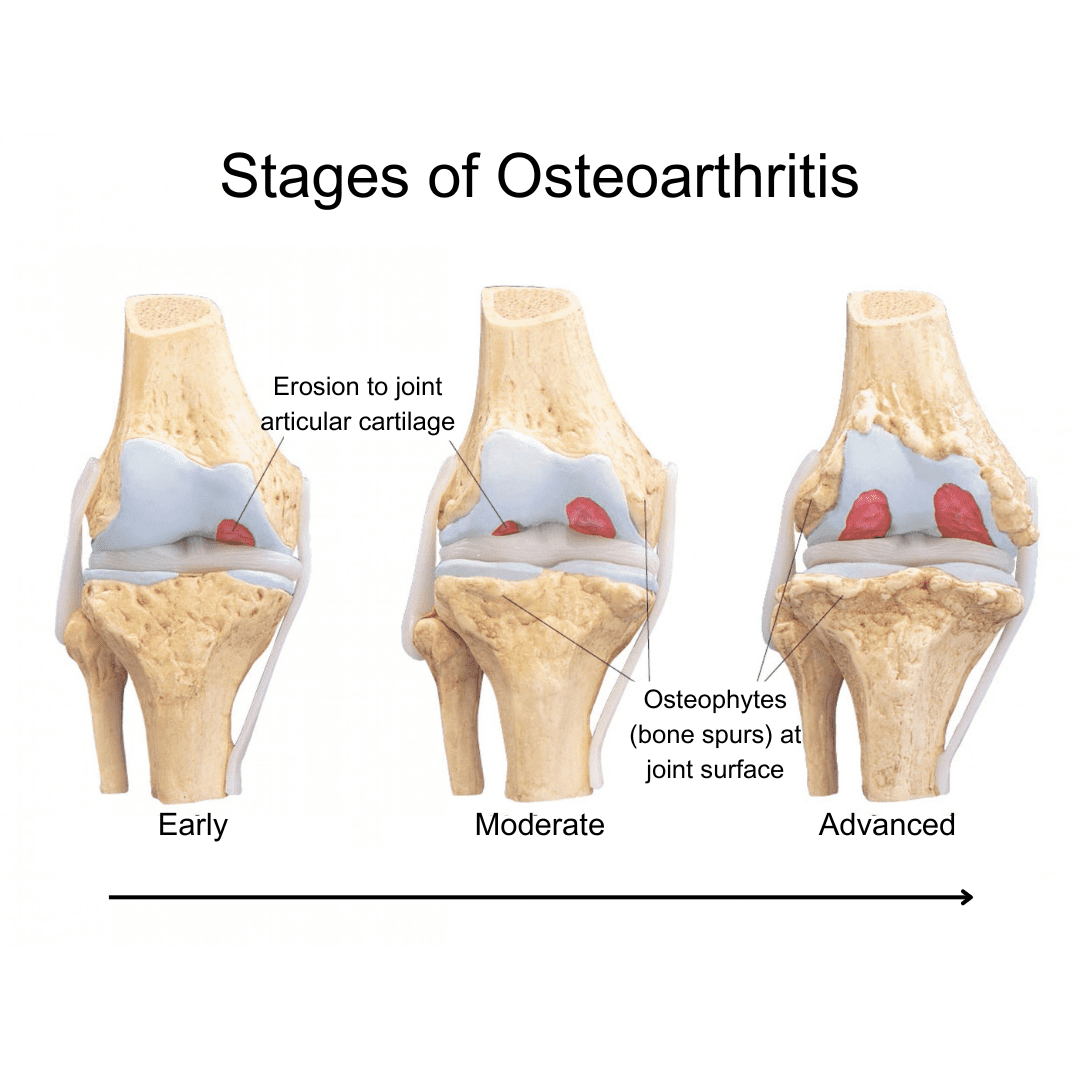
When the joint begins to degenerate, the cartilage on the joint surface may start to soften or develop pits and wear. The joint may also experience mild inflammation. Patients may feel knee pain when going up or down stairs, or walking on inclines. The joint may also feel slightly sore, red, swollen, and tight. During joint movement, an abnormal grinding or crepitus sound can often be heard.

Late-stage Symptoms of Osteoarthritis
When the degeneration becomes more severe, the cartilage may be worn down completely. This is accompanied by underlying bone erosion, ligament laxity, joint capsule instability, and inflamed and swollen synovium. The degenerated joint may become irregular and develop bone spurs (osteophytes).
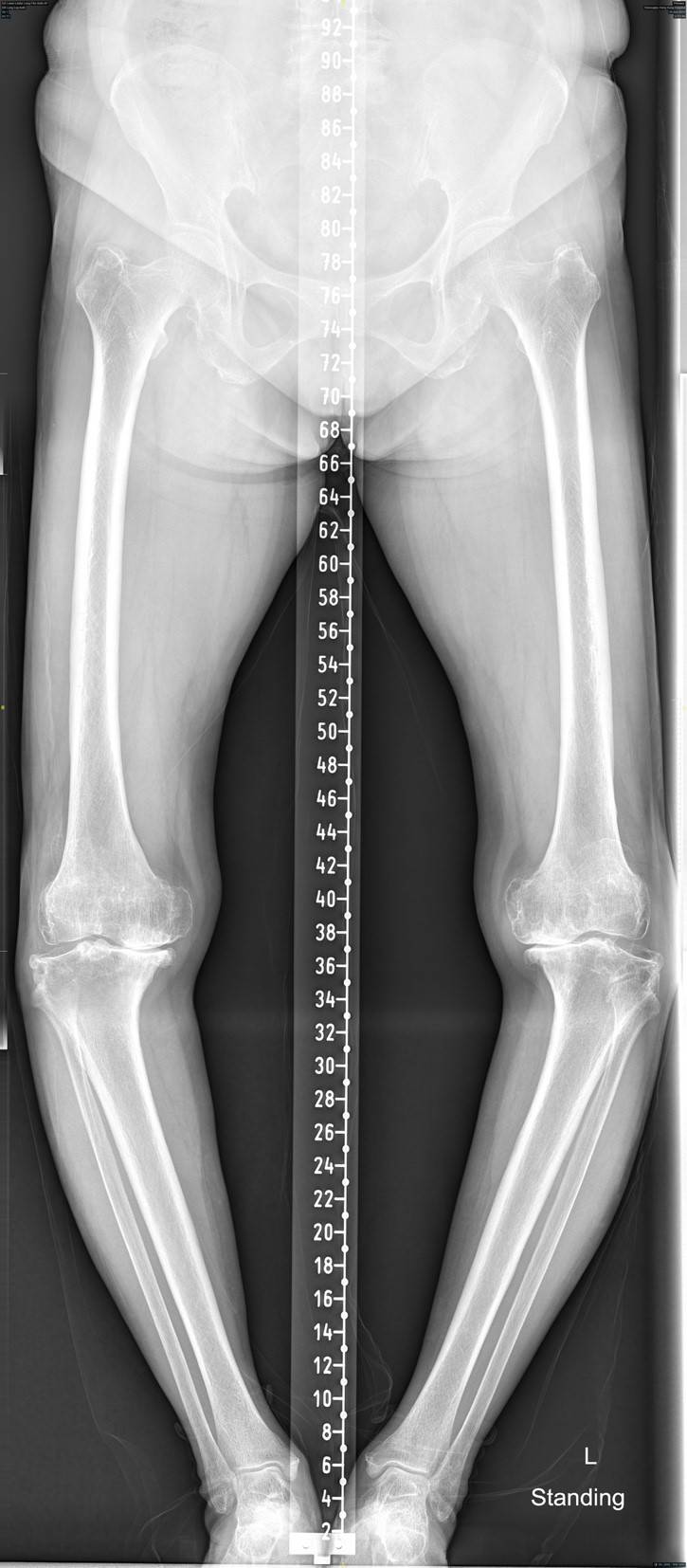
Patients may experience joint stiffness, inability to flex or extend, or develop deformity, resulting in "O-shaped feet". The range of motion of the joint is reduced, making it impossible to stand for long periods of time and causing weakness especially upon walking up stairs or squatting. Upon environment temperature change or upon movement, your joints will experience severe pain, making it difficult to move. These symptoms not only cause inconvenience in the patient's work and daily life, but also have the potential to impact their emotional well-being.

How is Osteoarthritis Diagnosed?
The doctor will first inquire about the duration and triggering factor of the patient's joint pain, as well as their medical and family history, in order to analyze the underlying causes. The doctor will also assess the severity of the osteoarthritis based on the patient's mobility and the frequency of pain medication usage.
After taking the history, the doctor will perform a comprehensive physical examination, focusing on the location of knee joint pain, patient’s ability to ambulate, presence of joint deformities, range of joint motion, strength of the lower limb muscles (e.g. quadriceps), joint instability, evaluation of ligament structure and tension around the joint, etc.
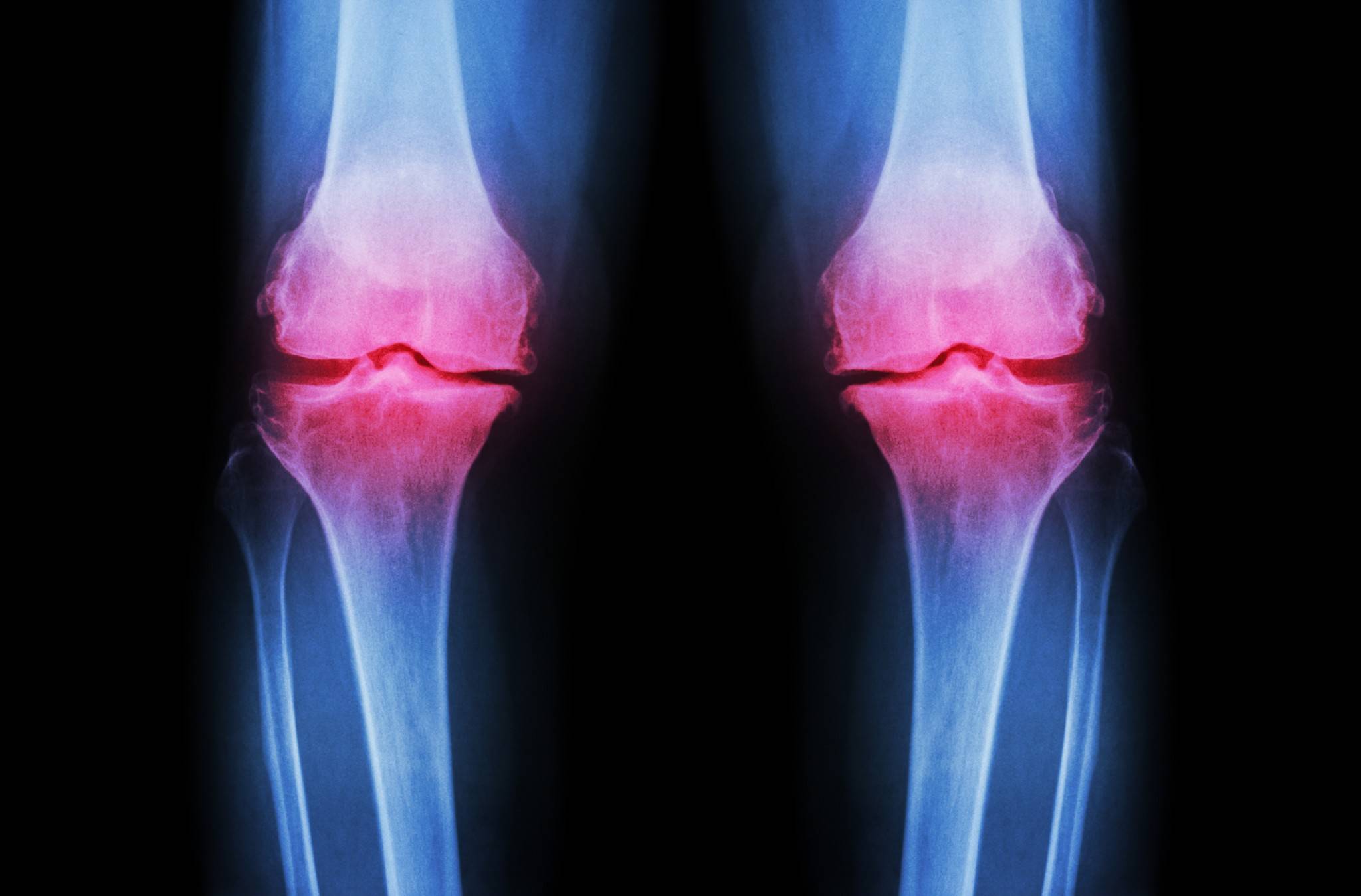
The doctor then will arrange patient to an X-ray imaging. On the X-ray, the doctor will specifically look for signs of joint space narrowing and soft tissue swelling. If you are already experiencing symptoms of joint pain, it is recommended to consult a professional medical doctor promptly to seek appropriate treatment.
4 Main Methods to Prevent Joint Pain
Through daily care, the symptoms of joint pain and arthritis caused by joint overdue can be effectively reduced. The following are the 4 main methods for preventing joint pain:
Moderate Exercise
Strengthening the muscles can provide stable support to the joints, reducing wear and tear. However, it's important to choose suitable exercises and avoid high-intensity activities that may lead to injury. Physical therapists can design exercises that help reduce joint pain. Many studies have confirmed the effectiveness of this method in improving symptoms.

Weight Control
Excess weight increases the burden on the joints, especially the knees and hips. Maintaining a healthy weight can effectively reduce joint stress and alleviate joint pain symptoms. Medical literature has shown that for patients with a BMI over 25, this method can effectively relieve pain.
Proper Posture
Poor posture increases joint pressure and may lead to joint pain in the long run. When standing, maintain a straight back. When sitting, provide lumbar support and avoid slouching or bending over.
Balanced Diet
Consuming adequate calcium, vitamin D, and other nutrients can help maintain healthy bones.
Treatment Options for Arthritis
Non-Surgical Treatments
Oral Medications
Non-steroidal anti-inflammatory drugs (NSAIDs) are the most common medications used to manage the pain associated with arthritis. They can effectively relieve symptoms, and guidelines from the American Academy of Orthopaedic Surgeons recommend their consideration as a treatment option.
Injection Treatment
Injections of hyaluronic acid (also known as "gel injections") can also be considered. Hyaluronic acid is a major component of the joint's synovial fluid, and it helps increase the viscosity and lubricating function of the synovial fluid. It is also an important part of joint cartilage, helping it retain water and provide compressive resistance.
Injecting hyaluronic acid directly into the joint space can have a lubricating effect on the joint. It may also stimulate the cartilage cells to produce new material to fill in the worn-down cartilage.


Autologous Protein Solution Injection (APS)
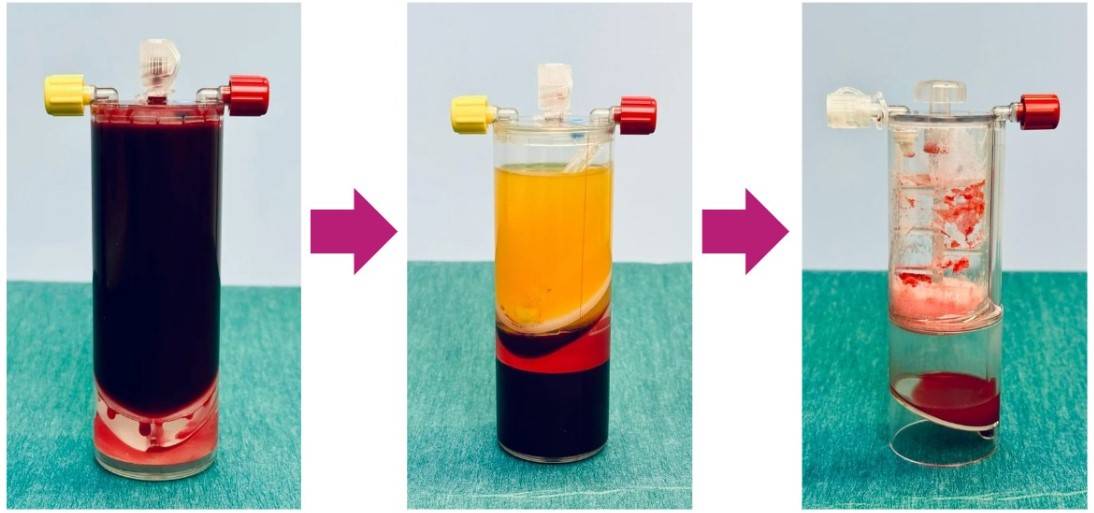
In recent years, the medical community has introduced high-concentration platelet (PRP) therapy for various joint and soft tissue issues. One innovative PRP treatment specifically targets knee joint degeneration and is known as "Autologous Protein Solution" (APS).
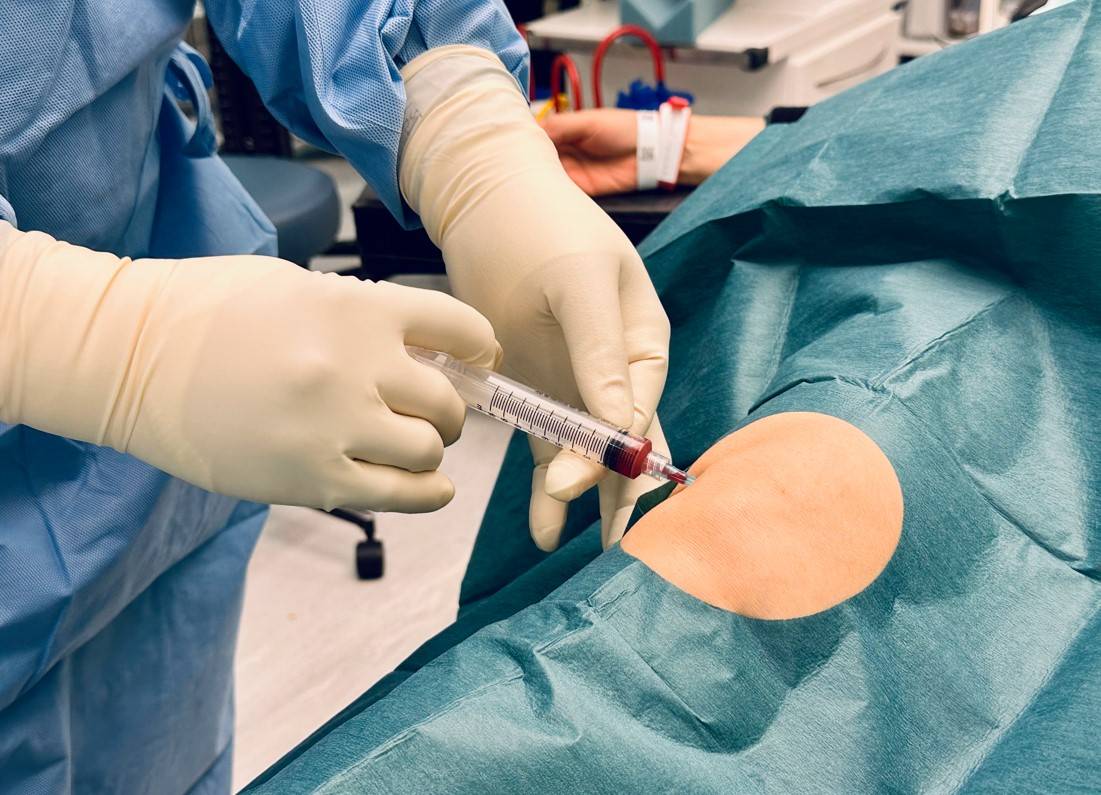
APS is a new injection therapy aimed at early to mid-stage degenerative knee arthritis. It involves a single injection process where approximately 60ml of blood is drawn from the patient. This blood is then centrifuged, concentrated, and processed to extract 3 to 4ml of a protein solution rich in growth factors and anti-inflammatory agents, which is precisely injected into the knee joint cavity.
The principle behind this therapy is to inject the patient's own high-concentration quality factors (anti-inflammatory and growth factors) into the joint, helping to reduce inflammation, alleviate pain, and repair damaged or degenerated cartilage. It is suitable for patients with early to mid-stage degenerative knee arthritis.
Exercise Therapy
Exercise therapy can be used to strengthen the muscles, thereby improving joint mobility. Additionally, cold therapy can be applied to help relieve joint pain and swelling.
Surgical Treatments
Doctors will typically evaluate the patient's medical history and severity of the condition, and then recommend different surgical treatment options. The common surgical procedures include arthroscopic surgery and joint replacement surgery.
- Arthroscopic Surgery
This minimally invasive procedure involves making two small incisions to insert an arthroscope. The surgeon can then remove any loose bone fragments or torn meniscus, and wash out the joint. This can help improve mobility for patients whose joint function is limited by loose fragments or torn cartilage. However, it does not address underlying cartilage degeneration. - Joint Replacement Surgery
The principle of joint replacement surgery is to replace the degenerated joint with an artificial prosthesis, in order to reduce pain and improve the patient's mobility. This can involve a total knee replacement or a partial knee replacement.
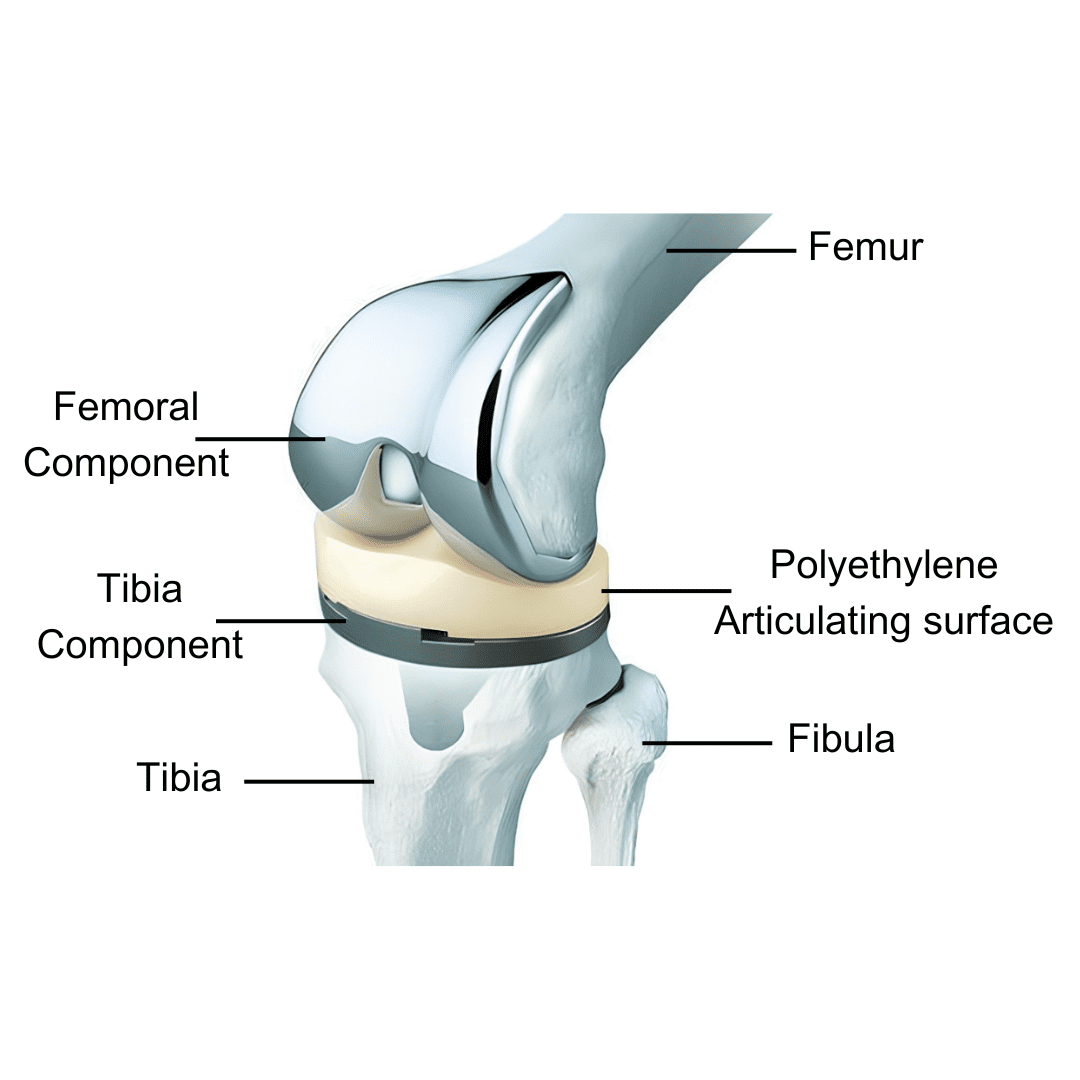
For patients with isolated single-compartment knee arthritis, a partial knee replacement is often recommended, as it involves a smaller surgical incision and less tissue trauma, allowing for a faster recovery. For advanced, widespread joint degeneration, a total knee replacement is usually advised.
In recent years, robotic-assisted total knee replacement has become more commonly performed. This allows the surgeon to precisely cut the bone and implant the artificial joint components, making the procedure more accurate, less invasive, and efficient.


















