Article was originally published in HK01.
Knee joints deteriorate with age, and when the cartilage is severely worn down, patients may need to undergo knee replacement surgery. Many patients are concerned about the trauma of the surgery and post-operative care. In fact, the surgery has undergone major improvements in three key areas: the robotic technology, new wound suturing techniques, and advanced wound dressings. These advancements enhance treatment efficacy and further reduce the risk of post-operative wound infection, helping patients regain mobility and quality of life.
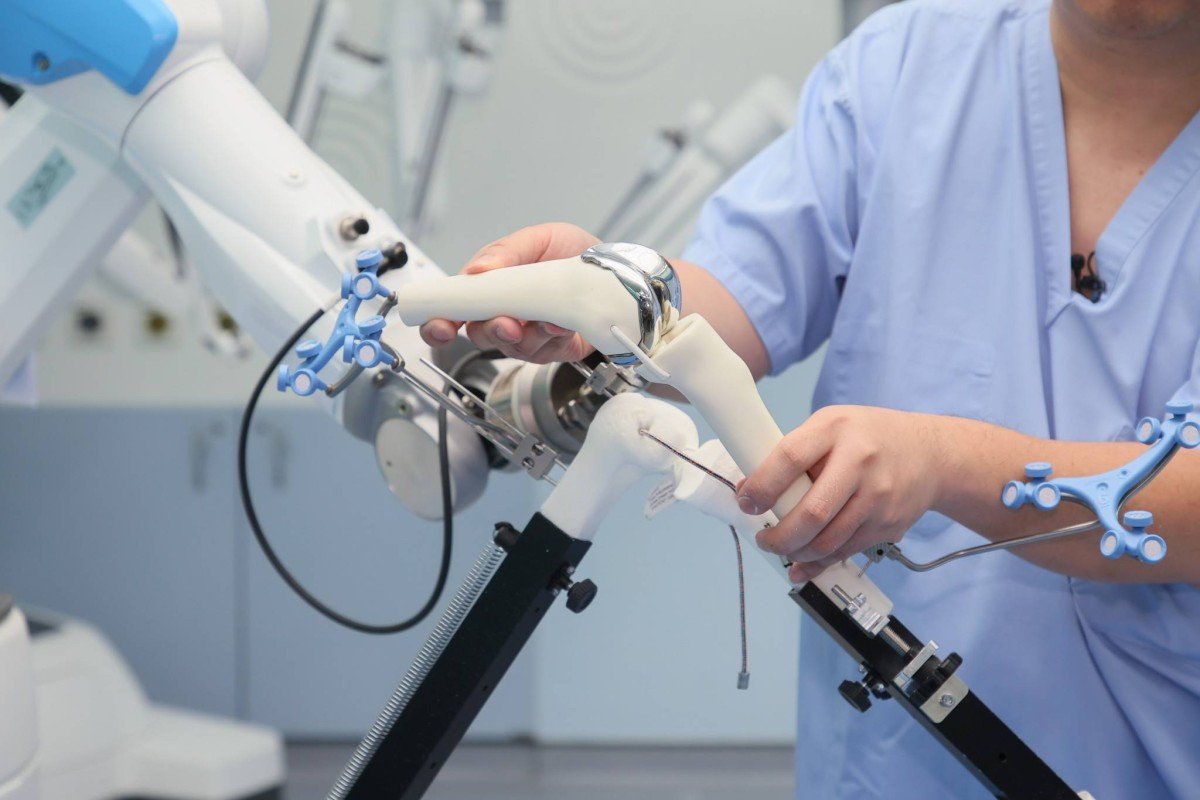
Knee replacement surgery involves removing the damaged knee joint and cartilage, and replacing them with an artificial joint made of metal and polyethylene on the femur and tibia, restoring normal knee joint range of motion. Orthopedic specialist Dr. Cheung Man Hong says that knee replacement techniques have been continuously improving over the past two decades, becoming more personalized. In recent years, robotic assisted knee replacement surgery (known as robotic surgery) has further enhanced the efficacy.
Dr. Cheung says that robotic surgery can perform bone cuts with greater precision, accurate to the millimeter. The ability to micro-adjust joint positions and accurately implant the prosthetic joint based on the soft tissue tension can reduce post-operative pain for patients. It is expected to become the mainstream approach for knee replacement surgery in near future.
New Generation Robotic Assisted Joint Replacement
This year, Hong Kong has introduced a new generation of robotic surgery, making the knee replacement process faster and more meticulous. Dr. Cheung says that in the past, robotic surgery required pre-operative planning, where patients had to undergo CT scans to input bone data and images for surgical planning. Now, this is no longer necessary - "Current systems only require X-ray scans, which saves the patient's time and medical costs, and avoids radiation exposure from the scans."
In addition, Dr. Cheung points out that each robotic surgical system is equipped with a specific joint prosthesis. The new generation system's component design is more ergonomic and stable, with fine adjustment of component size sizes to further improve surgical outcomes. The surgery time is also faster than the previous generation of robotic surgery, taking about an hour and a half, closer to traditional surgery duration. Around 90% of patients can get out of bed on the same day after surgery and do not require physical therapy upon discharge, allowing them to recover their quality of life faster. For surgeons, the learning curve is also shorter, with proficiency achieved after performing around 10 cases.
Non-Invasive Zipper Suturing Technique
Joint replacement surgery is a medium to major operation, with an incision generally 14 to 16 cm long that needs to be properly sutured until healing is completed. Dr. Cheung explains that traditional suturing methods usually involve stitches or staples. About five to six years ago, the medical community started using dissolvable stitches to suture wounds, which had the benefit of not needing to be removed, but the downside was that the foreign material in the body may not be optimal for healing. The latest non-invasive wound closure technique combines the advantages of traditional methods, helping the wound heal better.
Dr. Cheung says this technique was introduced to Hong Kong around two years ago. It involves directly applying a zipper-like device onto the wound and then tightening it. The benefits are that it does not require piercing the skin and there are no foreign objects left in the body. Patients can have it removed after two weeks, which only takes a few seconds.
Patients may be concerned about whether this "zipper" can adequately protect the wound. Dr. Cheung cites over a hundred local cases using this technique, and so far there have been no issues with wound rupture or instability, and scarring is also reduced. "Scarring is caused by external stimulation, but the zipper technique provides better protection with fewer external influences, so the risk of scarring is lower." He adds that this technique can be applied to any surgical incision.
Antimicrobial Dressings Reduce Post-Operative Infection, Good Water Resistance
After applying the "zipper", a dressing is still needed to protect the wound and reduce the risk of infection. Dr. Cheung points out that patients are very concerned about wound protection after surgery, such as fears of showering, water seepage, and bacterial infection, and hope to be able to walk comfortably as soon as possible.
In addition to making the patient's post-operative life more convenient, the dressing's most important function is to prevent bacterial invasion. If a postoperative infection occurs, the wound or surrounding area may become red, swollen and suppurate, and the patient may develop fever, chills and fatigue. The joint may also become painful again or have reduced range of motion.
For this reason, the materials used in dressings have also evolved. Dr. Cheung cites the example of the new generation of dressings, which combine multiple layers to achieve a waterproof effect and incorporate silver ion material. This allows the dressing to absorb wound exudates and bacteria, and the silver ions can then kill the absorbed bacteria, achieving an antimicrobial and preventive infection effect. He says that when the dressing is removed, the "zipper" can be pulled out at the same time, saving time, which is a good protective combination.
This article was written by Dr. Cheung Man Hong, an Orthopedic Consultant & Clinical Director Of Robotic Surgery (Joint Replacement) at Hong Kong Adventist Hospital – Stubbs Road.

















